By Dr. Karl Michel –
 Having trouble standing, walking or running? A great number of the population at some point in their lifetime will suffer from heel pain which often impede them from their daily activities. If you haven’t had to deal with it personally, just ask around. Chances are you know lots of people who can describe it in great detail: stabbing heel pain and agonizing steps followed by a frustratingly slow recovery. The two most common causes of this debilitating heel pain are usually Plantar Fasciitis or Achilles Tendinitis. The easiest way to figure out which one is causing your pain is by location. Generally speaking, if the pain is under your heel bone it is likely plantar fasciitis. If the pain is found at the back of the heel, in the achilles or toward the base of the achilles (the long cord that extends from your calf to your heel bone), then it is likely achilles tendinitis.
Having trouble standing, walking or running? A great number of the population at some point in their lifetime will suffer from heel pain which often impede them from their daily activities. If you haven’t had to deal with it personally, just ask around. Chances are you know lots of people who can describe it in great detail: stabbing heel pain and agonizing steps followed by a frustratingly slow recovery. The two most common causes of this debilitating heel pain are usually Plantar Fasciitis or Achilles Tendinitis. The easiest way to figure out which one is causing your pain is by location. Generally speaking, if the pain is under your heel bone it is likely plantar fasciitis. If the pain is found at the back of the heel, in the achilles or toward the base of the achilles (the long cord that extends from your calf to your heel bone), then it is likely achilles tendinitis.
Plantar Fasciitis is an overuse injury that affects the sole of the foot, creating pain along the plantar fascia as it connects to the heel bone. The plantar fascia is the band of tissue that supports the arch; it connects the heel bone to the base of the toes. When the plantar fascia is strained, it gets weak, swollen, and irritated or inflamed thus the term plantar fasciitis.
What are the signs and symptoms?
• Pain on standing, especially after periods of inactivity or sleep. People with plantar fasciitis often describe the pain as worse when they get up in the morning or after they’ve been sitting for long periods of time.
• Pain subsides, returns with activity. After a few minutes of walking the pain decrease, because walking stretches the fascia. For some people the pain subside but return after spending long periods of time on their feet.
• Pain related to footwear. This can be worse in flat shoes which offer no support, wearing non-supportive footwear on hard, flat surfaces puts abnormal strain on the plantar fascia to such an extent that the area becomes swollen or inflamed.
• Radiating pain to the arch and/or toes
• In later stages, pain may persist/progress throughout the day. This is particularly evident when one’s job requires long hours on the feet.
• Pain varies in character: dull aching, “bruised” feeling. Burning or tingling, numbness, or sharp pain, may indicate local nerve irritation
Some other potential causes of heel pain are:
• Severs disease (calcaneal apophysitis) – the most common cause of heel pain in child/teenage athletes, caused by overuse and repetitive micro trauma of the growth plates of the calcaneus (heel bone). Children aged from 7-15 are most commonly affected.
• Stress fracture – this is a fracture caused by repetitive stress, commonly caused by strenuous exercise, sports, or heavy manual work. Runners are particularly prone to stress fracture in the metatarsal bones of the foot. Can also be caused by osteoporosis.
• Tarsal tunnel syndrome – a large nerve in the back of the foot becomes pinched, or entrapped (compressed). This is a type of compression neuropathy that can occur either in the ankle or foot.
• Chronic inflammation of the heel pad – caused either by the heel pad becoming too thin, or heavy footsteps.
• Bone cyst – a solitary fluid-filled cyst (cavity) in a bone
• Problems with your gait – wrong posture when walking/running.
• Achilles tendon rupture – the tendon of the heel cord behind the ankle is torn.
Evaluation and Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot to determine your foot type, low vs. high arch. Throughout this process the surgeon will rule out all the possible causes for your heel pain other than plantar fasciitis.
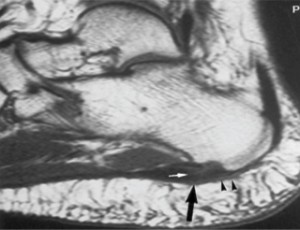
In addition, diagnostic imaging studies such as x-rays or other imaging modalities ultrasound or MRI may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Treatment
Treatment of plantar fasciitis begins with first-line strategies, which you can begin at home. Most heel pain patients respond to initial therapies within a relatively reasonable period of time:
• Stretching exercises. Exercises that stretch out the calf muscles help ease pain and assist with recovery.
• Avoid going barefoot. When you walk without shoes, you put undue strain and stress on your plantar fascia.
• Ice. Putting an ice pack on your heel for 20 minutes several times a day helps reduce inflammation. Place a thin towel between the ice and your heel; do not apply ice directly to the skin.
• Limit activities. Cut down on extended physical activities to give your heel a rest.
• Shoe modifications. Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia.
• Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
If you still have pain after several weeks, see your foot and ankle surgeon, who may add one or more of these treatment approaches:
• Padding and strapping. Placing pads in the shoe softens the impact of walking. Strapping helps support the foot and reduce strain on the fascia.
• Orthotic devices. Custom orthotic devices that fit into your shoe help correct the underlying structural abnormalities causing the heel pain.
• Injection therapy. In some cases, corticosteroid injections are used to help reduce the inflammation and relieve pain.
• Removable walking cast. A removable walking cast may be used to keep your foot immobile for a few weeks to allow it to rest and heal.
• Night splint. Wearing a night splint allows you to maintain an extended stretch of the plantar fascia while sleeping. This may help reduce the morning pain experienced by some patients.
• Physical therapy. Exercises and other physical therapy measures may be used to help provide relief.
Some other options includes: Minimally invasive procedures like ESWT (Extracorporeal Shock Wave Therapy), and Autologous Platelet Rich Plasma (PRP) injection.
When Is Surgery Needed?
Although most patients with heel pain respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you.
Long-term Care
No matter what kind of treatment you undergo for heel pain, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment.
How does one prevent heel pain? Some Helpful Tips
Prevention of heel pain involves reducing the stress on that part of the body.
Bare feet – when on hard ground make sure you are wearing shoes.
Bodyweight – if you are overweight there is more stress on the heels when you walk or run. Try to lose weight.
Footwear – footwear that has material which can absorb some of the stress placed on the heel may help protect it. Examples include heel pads. Make sure your shoes fit properly and do not have worn down heels or soles. If you notice a link between a particular pair of shoes and heel pain, stop wearing them.
Rest – if you are especially susceptible to heel pain, try to spend more time resting and less time on your feet. It is best to discuss this point with a specialized health care professional.
Sports – warm up properly before engaging in activities which may place lots of stress on the heels. Make sure you have proper sports shoes for your task.
INTEGRATIVE FOOT & ANKLE CENTER
Dr. Daniel Pero & Dr. Karl Michel
(561) 293-3439 | www.integrativefoot.com
Check Also
RejuvaNATION MedSpa: Elevating Men’s Health to New Heights
Embark on a Journey to Revitalize Your Vitality Rediscover the joy of a spontaneous sex …
 South Florida Health and Wellness Magazine Health and Wellness Articles
South Florida Health and Wellness Magazine Health and Wellness Articles




