 By midlife more than fifty percent of the population experiences significant episodes of low back or lumbar pain. Oftentimes, chronic low back pain leads patients to surgery of the lumbar spine. Unfortunately, ten to forty percent of the lumbosacral spine surgeries done for disabling pain culminate with recurrent or persistent pain. The numbers are so overwhelming that this condition has its own diagnosis. This condition is known as Failed Back Surgery Syndrome (FBSS).
By midlife more than fifty percent of the population experiences significant episodes of low back or lumbar pain. Oftentimes, chronic low back pain leads patients to surgery of the lumbar spine. Unfortunately, ten to forty percent of the lumbosacral spine surgeries done for disabling pain culminate with recurrent or persistent pain. The numbers are so overwhelming that this condition has its own diagnosis. This condition is known as Failed Back Surgery Syndrome (FBSS).
What does FBSS involve? Interestingly, even though a back surgery is considered “successful,” because the anatomic area was surgically “fixed,” the defining symptoms of FBSS, persistent back and/or leg pain, can occur. The pain and discomfort cause a major negative impact on the ability to manage everyday activities such as standing, lifting, and traveling.
MRI findings can lead to unnecessary surgery
With so much technological progress, how does this still happen? Sometimes surgery is done when it was never indicated. Surgery may be recommended based primarily on MRI findings. This involves performing surgery on a structure that looked bad on MRI, but was actually not the true cause of pain. While operating on one condition, another condition may be overlooked. A disc may be removed, for example, but the underlying instability, causing disc degeneration and stenosis is not addressed. Disappointing results and pain will often result.
Joint Instability — the Link to Sciatica and other Back Pain Conditions
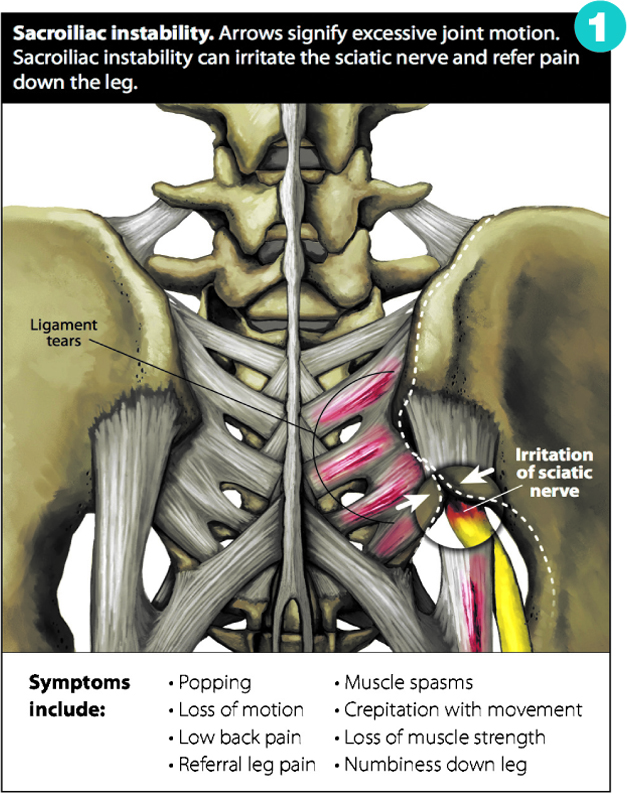
Back pain that goes down the leg, commonly referred to as “sciatica,” is an example of a common reason why people end up in surgery. If surgery is done to release the pressure on the sciatic nerve, but the patient complains of residual pain, this indicates that there are other structures causing the pain which were not addressed by the surgery. Pain that comes and goes or is worse in certain positions points to sacroiliac joint instability. (See Figure 1.)
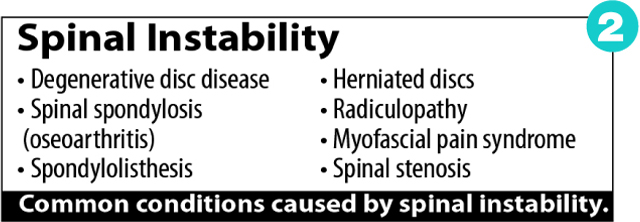
Fusion surgery may be recommended due to excessive movement, or instability, in the spine. The surgeon is looking to place artificial material to permanently fuse that area together, to keep it from moving. Once the joints are fused together, motion in the spine has to come from somewhere else, creating added stress on the sections above and below the spine.
One of the well-known long term effects is degenerative arthritis below and above the fusion. In numerous cases, this creates added back pain and arthritis after the surgery and a continued need for medical treatments. Regenerative Medicine options are available to stabilize the vertebrae without surgery.
Nonsurgical treatments for back pain
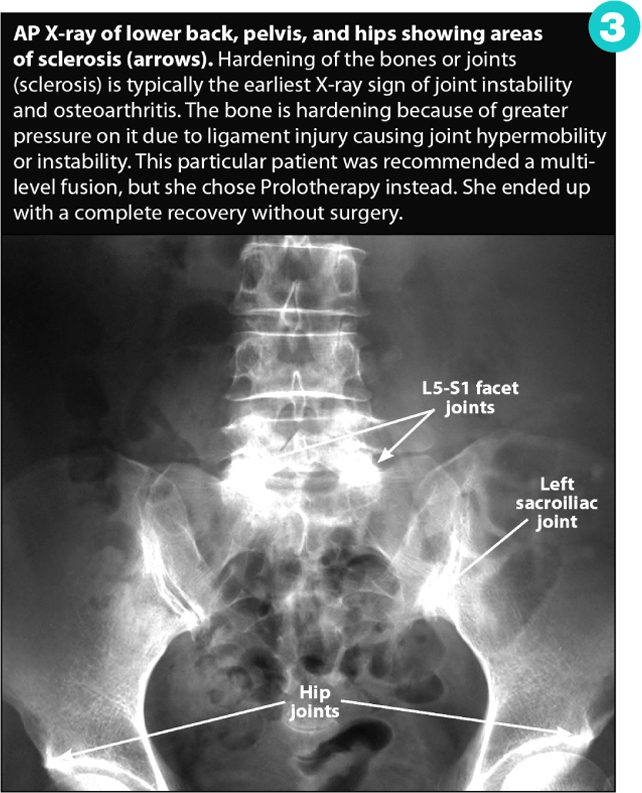
Regenerative Medicine refers to modalities that stimulate the body to repair itself, such as Prolotherapy, PRP and Stem Cell therapies. Our bodies have amazing regenerative capabilities and this can be harnessed to help degenerative conditions that show up on X-ray or MRI. (See Figure 3.) This is a novel approach because we are triggering the body to strengthen the tissue on its own, without the use of artificial hardware.
Prolotherapy Specialists:
Ross A. Hauser, MD.
Danielle R. Steilen, MMS, PA-C
Timothy L. Speciale, DO
Southwest Florida Location:
9738 Commerce Center Court
Fort Myers, FL 33908
(239) 303-4069
www.CaringMedical.com
Check Also
A Guiding Hand: Finding Compassion & Clarity in Life’s Toughest Moments
In life’s most difficult moments, finding a source of strength and guidance is paramount. For …
 South Florida Health and Wellness Magazine Health and Wellness Articles
South Florida Health and Wellness Magazine Health and Wellness Articles




