By Jerry Lerner, M.D. – Sierra Tucson Medical Director & Chief of Pain Medicine –
 Chronic pain is not the same as acute, simple pain. Studies performed with a functional MRI machine (fMRI) in recent years have helped us ro understand that the brain of a person in chronic pain works differently than a person who has new onset of pain. This is important to understand in order to help reduce the severity of pain.
Chronic pain is not the same as acute, simple pain. Studies performed with a functional MRI machine (fMRI) in recent years have helped us ro understand that the brain of a person in chronic pain works differently than a person who has new onset of pain. This is important to understand in order to help reduce the severity of pain.
When a healthy, comfortable person is placed in an MRI machine and given a painful stimulus, a localized area of the brain lights up. This area, known as sensory cortex, registers and identifies the sensation. However, if a person with chronic pain is placed in the MR I machine and provided with a painful stimulus, the picture is very different. Not only does the sensory cortex light up, but also other areas of the brain. One of these areas of the brain is known to be associated with strong emotions such as anger and fear. The other area deals with analyzing past experiences to help determine what to do in the present and to project into the future. This enlarged area of brain activation associated with chronic pain is very significant. Instead of just experiencing the painful sensation, the pain gets connected with the strong emotional center and with thoughts/regrets about the past and worries/ruminations about the future. One could say that a new pain (localized in the brain) is simple, objective pain, but that chronic pain (spreading into larger areas of the brain) is both pain and suffering. Anger, fear, past regrets, future worries that is the brain pattern of a person in chronic pain. It is far more distressing than the mere sensation of pain. This is, in part, why people who experience chronic pain are prone to depression, anxiety, and withdrawal from life. It also is partly why typical pain medications have a limited effectiveness with chronic pain. No pain reliever was designed to relieve pain along with worry, anxiety, depression, or grief.
Fortunately, there is an effective way to reverse the “brain spread” associated with chronic pain. Variously known as mindfulness, meditation, or the relaxation response, this very simple practice has been proven to reverse brain spread if practiced daily. fMRI studies have shown the brain to return to a normal state with as little as two months of daily practice. Research on mindfulness has confirmed that practitioners measurably reduce pain, anxiety, and depression.
If mindfulness was a pill you could rake, it would be the most successful medication on the market. There are many ways to practice mindfulness, or relaxation.
Following is a simple way to start:
Sit up in a relaxed position, as comfortable and supported as you can be. Close your eyes and begin to pay attention to your breath. Follow your breath as it enters your nostrils and enters your lungs, and follow it as the air leaves again. Continue to follow each breath in and out. No need to control or alter your breath, just pay attention to it. It is natural that from time to time your attention will wander. As soon as you become aware of this, simply bring your attention back to the breath. No need to judge yourself or strive for perfection.
Simply follow the breath, and when attention wanders gently return mention to the breath. Practice this for 10 to 30 minutes once or twice daily and within 8 weeks your pain and suffering will feel less intense, and your mood will feel improved.
Other benefits of a mindfulness practice can include improved sleep, better digestion, and lower blood pressure.
Adding mindfulness to other healing practices for your pain such as regular, safe exercise; healthy diet; competent body work; and appropriate medical support will have you, well on your way to feeling back in control of your life.
For those people who are struggling to find their way back to life from chronic pain and for whom good outpatient treatment and self-care has not been enough to turn things around, I strongly urge you to check our the Sierra Tucson Pain Management Program, a residential program designed to address all aspects and complications of chronic pain.
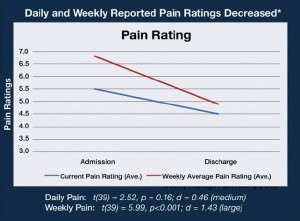
In a preliminary study conducted during 2011 and 2012, pain-related quality-of-life measures were collected from 41 patients in Sierra Tucson’s Pain Management Program upon Admission and Discharge. The patients in this sample completed a series of pain-related and health-related quality of life scales from the PROMIS initiative, and other validated pain functioning measures. In addition to the graph below showing how pain ratings decreased daily and weekly during treatment for chronic pain, Sierra Tucson invites you to see more outcomes research data at www.SierraTucson.com or to call 8008424487 for more information.
Check Also
WHY DO I FEEL SO TIRED ALL OF THE TIME, AND NOTHING WAKES ME UP?
By Renee Chillcott, LMHC When it comes to a feeling we can’t tolerate and want …
 South Florida Health and Wellness Magazine Health and Wellness Articles
South Florida Health and Wellness Magazine Health and Wellness Articles